Friendly Note: FreeJupiter.com shares general info for curious minds 🌟 Please fact-check all claims—and always check health matters with a professional 💙
It turns out that your brain might not be the only organ pulling the strings when it comes to depression. According to a new study from Harvard scientists and the Broad Institute, certain gut bacteria may be quietly stirring up inflammation that messes with your mood—and it might all start with a sneaky chemical found in everyday products.
A Gut Feeling About Depression
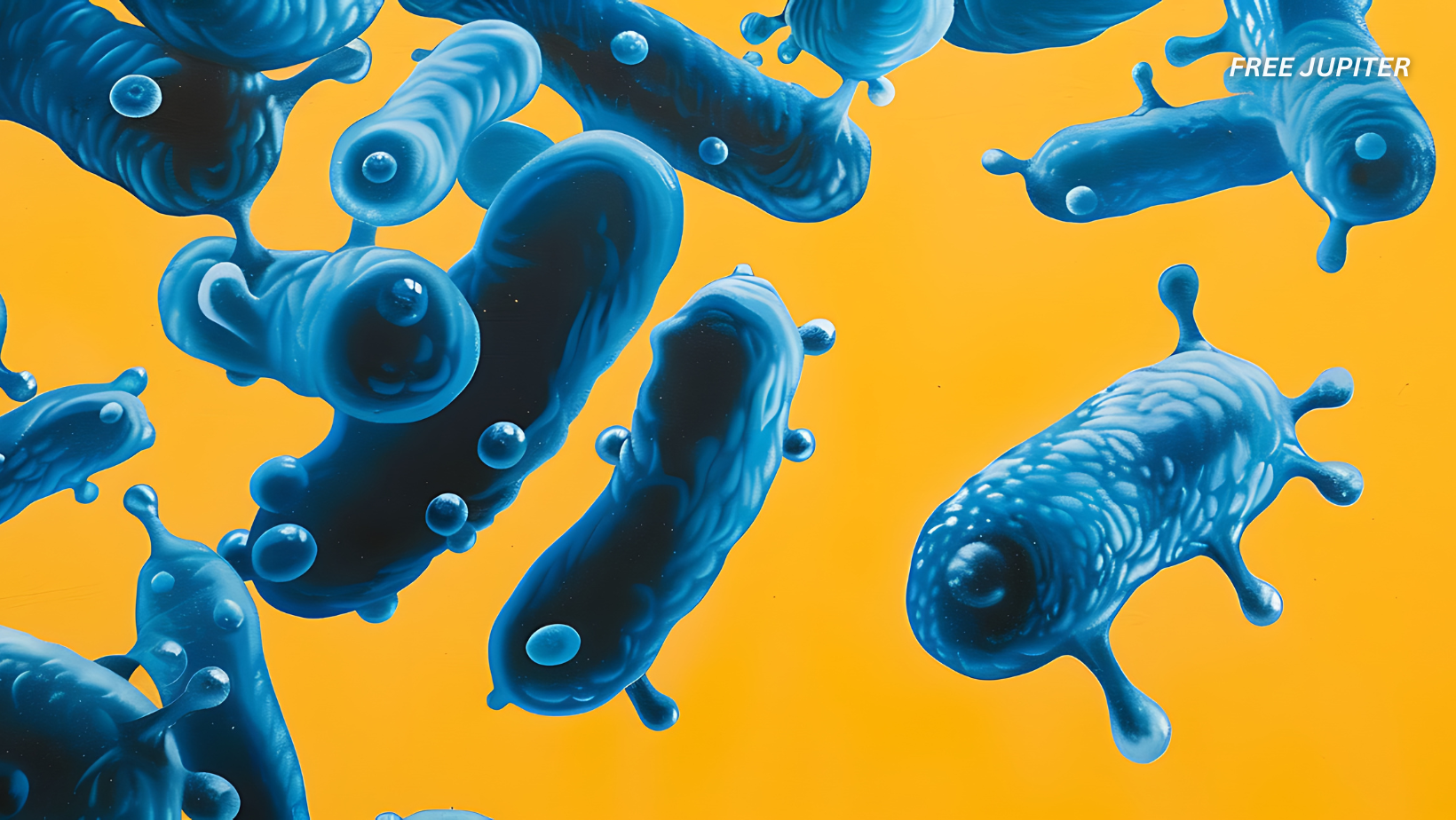
For years, researchers have been talking about the “gut-brain connection,” suggesting that the microbes living in your digestive system can influence mental health. Now, scientists have zoomed in on one particular troublemaker: Morganella morganii, a microbe already known to be involved in health problems like type 2 diabetes and inflammatory bowel disease.
The research team wanted to understand how this bacterium could be contributing to depression. What they found was unexpectedly complex—and strangely elegant.
The Dirty Work of a Tiny Chemical
Here’s where things get quirky. This gut bacterium, M. morganii, can tinker with a common chemical called diethanolamine (DEA). You may have never heard of DEA, but it’s lurking in your life more than you realize. It’s used in lots of products—like shampoo, soap, and even some industrial cleaners. Most people are exposed to it regularly, often without knowing.
Now for the twist: M. morganii absorbs this DEA and uses it to make special fat-like molecules. These altered fats look a lot like natural molecules in your body, but because of that tiny swap with DEA, they behave very differently.
How These Molecules Trigger Inflammation
The fat molecules created by M. morganii—scientists call them MmDEACLs (yes, it’s a mouthful)—don’t just sit around quietly. Instead, they wake up your immune system. More specifically, they poke two immune sensors in your body, called TLR1 and TLR2.
Imagine these sensors as tiny alarm systems. When triggered, they scream, “Something’s wrong!” and your body responds by releasing a substance called interleukin-6 (IL-6). This molecule fuels inflammation—a normal defense mechanism, but not one you want running 24/7.
Read more: Chewing Gum Sets Off Microplastic Bombs In Your Mouth, Study Reveals
IL-6 and Depression: What’s the Link?
Here’s why IL-6 matters in this story: high levels of it have been consistently found in people with depression. It’s not just a side effect—it seems to be a key player. IL-6 can interfere with how brain cells talk to each other, especially in areas linked to emotion and memory, like the prefrontal cortex and hippocampus.
So if your gut bacteria are churning out DEA-altered fats that constantly trigger IL-6, it’s like your immune system is quietly fueling a fire in your brain. Over time, that low-grade inflammation may start affecting your mood.
Tiny Tweaks, Big Consequences
What amazed the scientists is how picky the immune system can be. Small tweaks in the shape of these molecules—like whether they have a tiny “double bond” in their fat chains—made a big difference in how strongly IL-6 was released. That means our bodies are surprisingly good at sensing microscopic changes in chemical structure.
It also means M. morganii isn’t just passively floating around in your gut. It’s doing chemistry—advanced, sneaky chemistry that changes how your immune system behaves.
Why This Study Is a Big Deal
This research does more than just link gut bacteria to mood disorders. It explains how the link works on a molecular level. That’s a huge step forward.
Before this, most talk of the “gut-brain connection” was based on vague correlations. Now we’re starting to uncover the actual biological chain reaction: pollutant + gut microbe = immune response = inflammation = depression (for some people, at least).
That’s not just fascinating—it’s useful. If we can identify people whose depression is fueled by this specific process, it opens the door to more targeted treatments.
What This Means for Mental Health
If this theory holds up in larger studies, it may reshape how we think about depression. It suggests that for some individuals, their symptoms may have more to do with an overactive immune system than anything going wrong inside their brain itself.
In those cases, traditional antidepressants may not be enough—or even the right tool. Anti-inflammatory therapies, or even treatments targeting the gut, could end up being more effective.
It also means that seemingly harmless exposure to certain chemicals in the environment could be tipping the scales toward poor mental health.
Read more:You Are A Wise And Old Soul If You Were Born On These Dates: Experts
A New Way to Spot (and Possibly Treat) Depression
The researchers believe that the DEA-altered fats could be used as “biomarkers”—clues in the body that help identify which patients might have depression tied to this immune response. That could make it easier to diagnose and treat this form of depression more precisely.
The team also plans to look into other gut bacteria to see if they’re up to similar tricks. If M. morganii is doing this, there’s a good chance other microbes are too.
Pollution, Bacteria, and Brain Health
This study is a striking example of how interconnected our bodies are with the world around us. A chemical used in soap ends up inside our guts. There, a bacterium hijacks it and transforms it into a molecule that messes with our immune system. And somewhere down the line, this could alter how we feel, how we think, and how we see the world.
While more research is needed to fully understand the ripple effects, this discovery adds a new layer to the story of mental health. It shows that pollution isn’t just bad for the environment—it could also be quietly affecting our emotions through backdoor routes in the gut.
The Bottom Line
So, could your depression be coming from your gut instead of your brain? For some, the answer might be yes. A single gut microbe, teamed up with a common chemical found in daily products, may be nudging the immune system in ways that subtly—or not so subtly—impact your mental health.
This study doesn’t offer a magic cure, but it does offer a fresh perspective—and one more reason to take the gut-brain connection seriously.
Your Gut Might Be Talking to Your Brain—Through Electricity, Not Just Chemicals
When we think about the brain and gut “talking,” we usually picture chemicals bouncing around, hormones sending messages, and maybe a growl reminding us it’s lunchtime. But what if the gut also has something a bit more… electric to say?
That’s exactly what researchers are beginning to uncover: that the gut might be sending direct electrical signals to the brain—and it could change how we understand everything from digestion to mood.
Read more: The Kinds Of Proteins You Should Eat Every Week, According to a Dietitian
Shocking Revelations from the Gut
Scientists have long known about the vagus nerve, the superhighway of communication between the gut and the brain. It carries information back and forth, often in the form of neurotransmitters or hormones. But recent studies suggest that certain gut cells—called enteroendocrine cells—might be doing more than just releasing hormones. They might actually act like neurons, firing off electrical impulses.
In other words, your gut may not just be feeling things. It might be thinking things, too.
The Gut’s Tiny Electricians
These enteroendocrine cells were once thought to be simple, slow hormone factories. But researchers noticed something odd: these cells could form direct connections with nerve fibers, and they could respond in milliseconds—not minutes—to what’s going on inside the gut.
Digested food, bacteria, and even pollutants can spark these cells into action. In turn, they can stimulate the vagus nerve with almost neuron-like precision. And just like that, your brain gets the message—fast.
This discovery is still fresh and somewhat controversial, but it offers a new layer of complexity to the gut-brain axis. It also raises fascinating questions about how our bodies respond to external stimuli in real time.
From Food to Feelings
Why does this matter? Because if these gut signals influence the brain so directly, they may be involved in emotional responses, decision-making, or even mood swings. Imagine that: your breakfast isn’t just fueling your body, it’s changing how you think or feel by zapping your brain through gut neurons.
It could also explain why certain foods, gut microbes, or environmental chemicals like diethanolamine (as found in the previous study) have such a profound effect on mental health. They might not just be triggering immune responses—they could be sparking gut electricity that jumps straight to the brain.
Rethinking the Gut-Brain Story
This research is still evolving, but it suggests we may have been underestimating the gut for decades. Rather than being a passive partner to the brain, the gut might be more like a co-pilot—quick, responsive, and sometimes moody.
And in the long run, that could change how we approach mental health, food science, and even how we treat neurological disorders.
After all, the next breakthrough in understanding depression, anxiety, or brain fog might just come from where you least expect it—your gut’s electrical whispers.
Disclaimer: The information in this article is for general informational purposes only and is not medical advice. We are not doctors, and this website is run as a family hobby project. Always consult a qualified healthcare professional before making decisions about your health. Please fact-check any claims and use this content as a starting point, not a substitute for professional guidance.