Type 1 diabetes has long been one of those chronic conditions that modern medicine could manage but not quite cure. People with this autoimmune disease must vigilantly monitor their blood sugar levels and give themselves insulin, often multiple times a day. It’s not just inconvenient—it’s a constant, lifelong burden. But a recent breakthrough is giving millions of people reason to hope that their daily dance with needles and glucose monitors might one day come to an end.
In a clinical trial that’s already making waves in the medical world, researchers have discovered a way to potentially restore insulin production in people with Type 1 diabetes. Yes, you read that right—restore. The hero of the story? Stem cells.
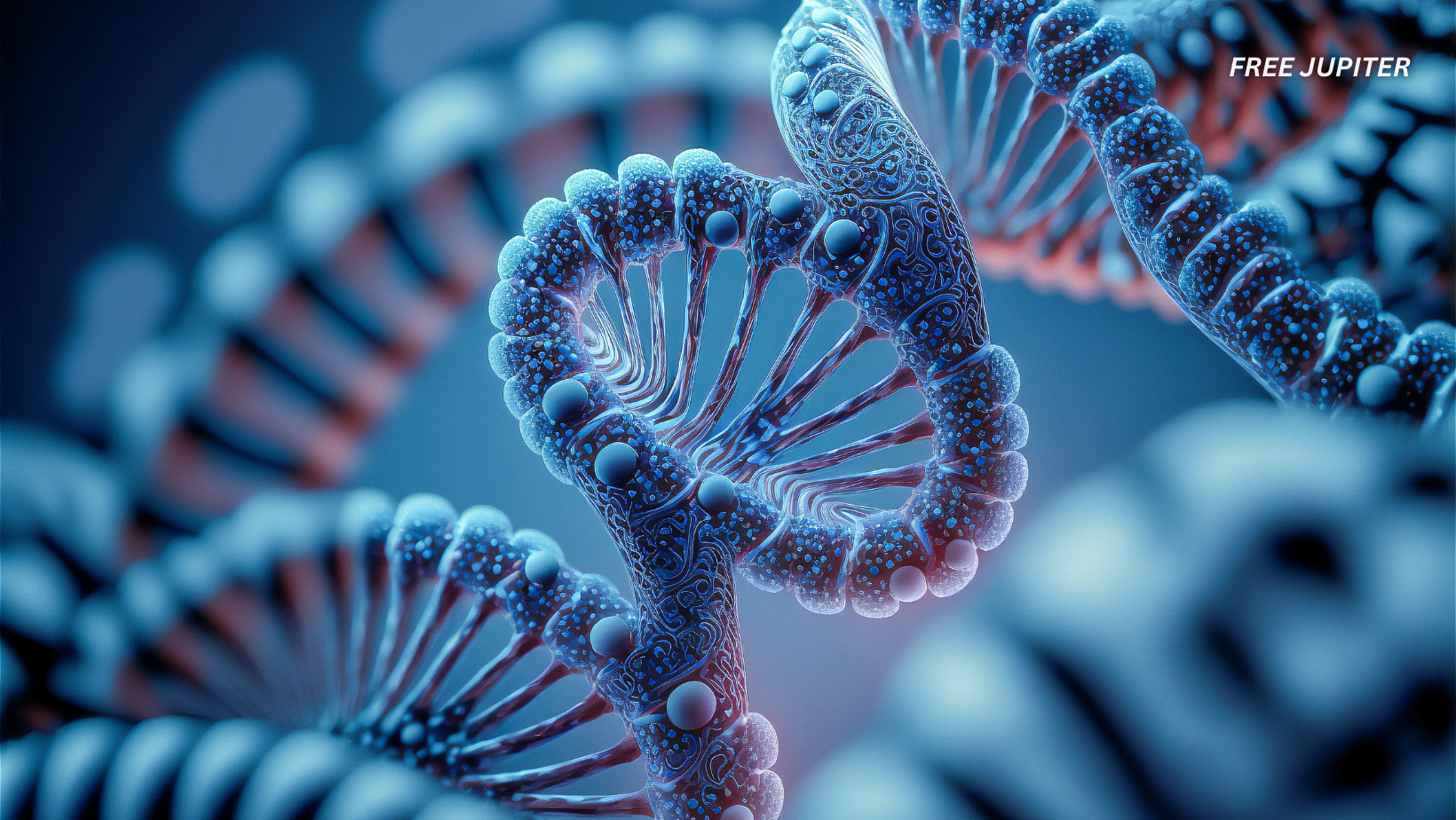
Stem Cells: Nature’s Building Blocks
Before diving into the heart of the discovery, let’s pause for a moment to understand what makes stem cells so magical. These tiny powerhouses are like blank slates. They can develop into many different types of cells—brain cells, skin cells, even insulin-producing islet cells in the pancreas. Scientists have long dreamed of harnessing stem cells to regenerate or replace damaged tissues in the body. Now, that dream may be turning into a reality.
The Trial That Changed Everything
The recent study involved 12 participants diagnosed with Type 1 diabetes. These individuals were infused with a special batch of pancreatic islet cells that had been grown from stem cells in a lab. The technique, officially called zimislecel, was developed by Vertex Pharmaceuticals, a biotech company making a name for itself in regenerative medicine.
Led by Dr. Trevor Reichman, a transplant surgeon at the University of Toronto, the trial aimed to see whether these lab-grown islet cells could survive inside the body and function like the real deal—producing insulin naturally and on demand.
Spoiler alert: it worked.
Read more: Doctors Say You Need to Know A Few Things Before Starting a GLP-1
One Year Later: Results That Stunned the Experts
Fast-forward a year after the treatment, and the outcome was nothing short of astonishing. Out of the 12 participants, 10 were able to stop using insulin completely. That means no more injections, no more insulin pumps—just their own bodies doing the job again, like before the disease struck.
Even the remaining two participants saw significant improvements in how their bodies handled blood sugar, suggesting that the treatment was beneficial even when it didn’t lead to full insulin independence.
What’s particularly promising is that the new islet cells didn’t just dump insulin randomly into the bloodstream. Instead, they behaved like native pancreatic cells—responding to changes in blood sugar and producing just the right amount of insulin at the right time. That level of precision is vital, especially in a condition where too much or too little insulin can be dangerous, even life-threatening.
How the Therapy Works
The zimislecel therapy works by introducing pancreatic islet cells—specifically, the kind that produce insulin—back into the body. These aren’t donor cells, which are limited and often require waiting lists. Instead, these were manufactured from pluripotent stem cells, which can be grown indefinitely and tailored to suit each patient’s needs.
The islet cells are infused directly into the liver, where they find a cozy spot to settle and start making insulin. This method has been used before with donor cells, but using lab-grown cells opens the door to a scalable and potentially universal treatment.
However, there is a catch.
The Role—and Risk—of Immunosuppressants
Because the immune system tends to treat any foreign cells as intruders (even ones trying to help), patients undergoing this therapy must take immunosuppressive drugs. These medications prevent the body from rejecting the implanted islet cells.
While the stem cell infusion itself caused no serious side effects, the immune suppression part isn’t risk-free. These drugs can reduce kidney function, increase vulnerability to infections, and in some cases, interfere with overall immune response. So while patients were able to stop insulin therapy, they had to trade one set of medications for another—at least for now.
Read more: Anti-Aging Tech Millionaire Tries Anti-Aging Drug—Ends Up Aging Even Faster
Tragedy Along the Way
Not all outcomes of the trial were celebratory. Two participants tragically passed away during the study period, though their deaths were determined to be unrelated to the stem cell therapy. Still, their passing is a stark reminder that medical research often unfolds in complex, unpredictable ways. Every success is hard-won, and each step forward comes with both hope and humility.
What This Means for the Future
Following the positive results, the therapy is now advancing to Phase 3 clinical trials—the last major hurdle before it can be approved for widespread use. This next stage will involve a larger group of participants and more rigorous testing to ensure the treatment works consistently and safely.
If successful, this stem cell-based approach could completely transform how we think about treating Type 1 diabetes. No longer would people have to rely on daily management tools. Instead, they could receive a single infusion and regain natural insulin control, possibly for years.
And because the islet cells are derived from stem cells (rather than human donors), the therapy can potentially be scaled to treat millions—something traditional transplantation methods could never achieve.
A Potential Cure—But Not Quite Yet
Calling it a “cure” might still be a bit premature. After all, patients still need immunosuppressants, and long-term outcomes are still being studied. However, the therapy brings us the closest we’ve ever been to reversing the effects of Type 1 diabetes, rather than just managing them.
It’s a massive step in the right direction—and one that builds on decades of research in stem cell science, immunology, and transplantation.
A Global Impact
Currently, around 8.4 million people worldwide are living with Type 1 diabetes, according to recent estimates. In many parts of the world, access to insulin is limited or unreliable. A therapy like this—once proven safe and scalable—could be nothing short of revolutionary.
Not only could it improve quality of life for millions, but it could also dramatically reduce the long-term health complications linked to diabetes, such as nerve damage, vision loss, kidney disease, and cardiovascular issues.
Read more: Injectable Hydrogel Literally Found to Increase Bone Density by Up to 5x, Study Shows
Final Thoughts: The Sweet Sound of Progress
Every once in a while, science stumbles across something truly game-changing—and this may be one of those times. By turning stem cells into functional insulin-producing cells and giving them a home inside the body, researchers have come closer than ever to restoring what Type 1 diabetes takes away.
Yes, challenges remain. Immunosuppression, costs, regulatory approvals, and long-term follow-up all need to be addressed. But for now, the simple fact that 10 people can live without insulin for the first time in years speaks volumes.
It’s not just about managing disease anymore. It’s about reversing it.
And that’s a future worth believing in.